The novel coronavirus requires a novel response.


In the fight against a global pandemic, HCA Healthcare’s scale offers many advantages. With approximately 280,000 dedicated colleagues, our collective know-how has fueled a number of innovations that benefit patients and caregivers.
“There’s so much talent,” says Kristy Frazier, MBA, BSN, RN, CSSM, clinical director of surgical services for the Clinical Services Group (CSG). “It’s great that they can come up with innovative ways that are safe for [everyone].”
The mindset that drives innovations reflects our core mission, says Dr. Michael Schlosser, National Group chief medical officer and vice president of clinical excellence and surgical services. “As a learning health system, we use our data to conduct research and create innovative tools that improve patient outcomes.”
Pre-intubation and intubation tents
The spread of the coronavirus causes concern that certain procedures such as intubation (insertion of a breathing tube) and extubation (removal of a tube) can put anesthesia providers and others at greater risk for infection.
“We know that COVID-19 is transferred from one person to another, or one surface to another, through aerosolization,” says Sandra Garrett, RN, MSN, CNOR, assistant vice president for surgical services for CSG. “We have procedures considered very high risk for that aerosolization, so we have to take more extreme [safety] measures.”
To limit potential exposure during airway manipulation, anesthesia providers have developed several devices to reduce aerosolization. One is an intubation box created by the staff at TriStar Centennial Medical Center in Nashville, Tenn.
Our telehealth visits grew tremendously and the patient response has been fantastic. I feel blessed to offer this option for patients and am proud to work for a healthcare organization so dedicated to advancing technology and always doing right by the patient.— Dr. Rachel Hailey, MD, HCA Midwest Health, Overland Park, Kan.
Made from clear Plexiglas, the large box goes over the patient’s head, with holes allowing anesthesia providers to place their hands inside to perform intubation or extubation.
“I’m amazed at all the ideas from the different staff members that just started flying at us,” says Sandra. “They’re actually moving quicker than we can give them approval to do so. Typically, healthcare initiatives don’t move that fast.”
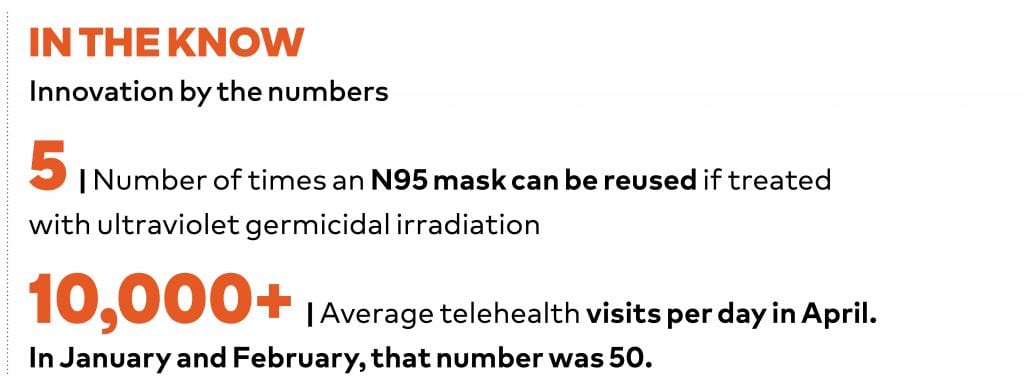
PPE sanitation
Healthcare professionals have relied heavily on personal protective equipment (PPE) during the pandemic. Medical masks—particularly the N95 model—have been a key tool. The well-documented global shortage of masks, however, required our facilities to get creative.
One solution, says Sandra, was reprocessing the masks to allow multiple use. “We have several facilities that implemented a pilot using ultraviolet germicidal irradiation, or UVGI.”
She says a team visited the Xenex company to learn about the process. Part of the training was to test the masks to ensure they fit after they were sanitized, since there was very little information on using UVGI, Sandra explains.
“The team, including nurses, wanted to provide assurance that this method would not compromise the integrity of the mask. Since the successful trial, they’re able to reprocess several hundred masks per day, allowing masks to be reused up to five times.”
Front-line hospital staff also need face shields, goggles and PAPR (Powered Air Purifying Respirators) shields and hoses, says Sandra. Like masks, these critical items have been in short supply. Sterile Processing Department staff members have stepped up to take on reprocessing this gear.
Telehealth
The pandemic has turned the “regular” practice of medicine upside down. However, patients who don’t have COVID-19 still need to be seen and still expect the usual high-quality care. The rapid expansion of telehealth medicine across our network allows caregivers to provide clinical excellence at more than 2,000 sites of care, says Christopher Northam, vice president of Telehealth Services. The system includes an app-based program to screen for COVID-19 symptoms through a remote monitoring partner, Vivify Health.
HCA Healthcare teams scaled this technology across more than 180 hospitals in less than seven days and (as this publication was going to press) had monitored more than 20,000 patients and colleagues. Those teams also added more than 3,000 telehealth endpoints so hospital clinicians can round on patients and finish consultations without entering patients’ rooms, preserving critical PPE.
HCA Healthcare teams also enabled telehealth capabilities for more than 6,000 physicians to provide continuity of care for primary and specialty care practices. Those physicians scaled from an average of 50 telehealth visits daily in January and February to more than 10,000 daily in April.
“Telehealth allows a patient to get much-needed care while staying safely at home,” says Gwen McCoy, assistant vice president of Telehealth Operations. “For those with a chronic illness, seeing his or her physician during this pandemic gives patients a welcomed virtual ‛house call.’”
Dr. Jeffrey S. Guy, MD, MS, MMHC, vice president of Emergency, Trauma and Critical Care Services, describes telehealth as “not a technology but a program of care,” emphasizing patient safety. “Our telehealth COVID-19 monitoring program uses a technology to connect patients and colleagues to clinicians who monitor their condition daily and, when needed, navigates them to a site of care. We’re able to stay connected to our medically fragile patients during a time when they feel vulnerable and anxious. Telehealth helps to prevent an ‛avoidable surge.’”
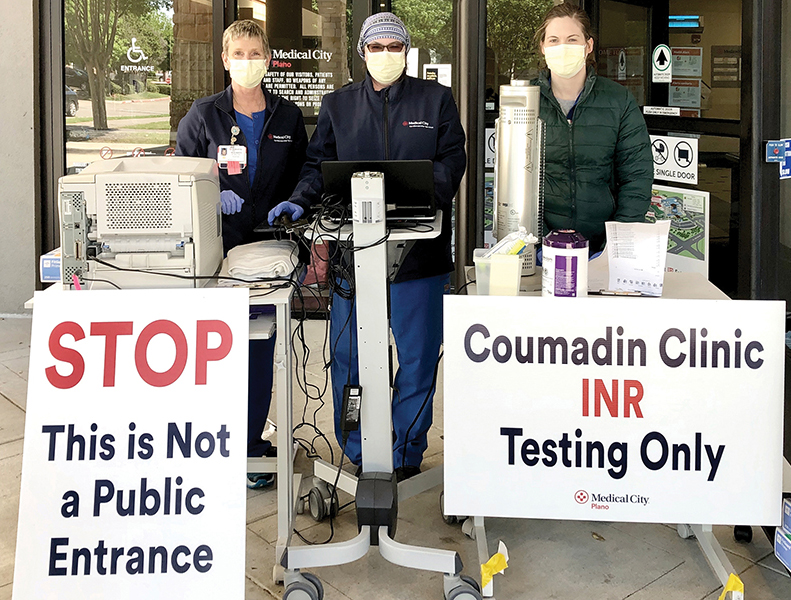
Drive-up Service at Medical City Plano (from left): Maureen Wilkerson, BSN, RN, CCRN; Jeanne Cross, BSN, RN, BC-N; Haley Franco, BSN, RN
Drive-through convenience
Since people with preexisting conditions are at high risk for infection, Medical City Plano in Texas launched a drive-up service allowing Coumadin and heart failure patients to be seen right in their car.
“The team is waiting outside with kits for lab draws and any vitals,” says Tammy Bauer, assistant vice president of Cardiovascular Services at Medical City Healthcare in Dallas. “For heart failure patients who need more than labs, after completing lab work, they’re sent home and the rest of the visit is managed using telehealth technology.”
COVID-19 “calculator”
With the capacity of the U.S. healthcare system challenged like never before, Michael is focused on measuring that capacity, which he says is where our organization can be most influential: determining “the number of cases that our system can handle without becoming overwhelmed.”
To aid in that effort, HCA Healthcare developed a COVID-19 “calculator.” It combines variables such as transmission estimates, average “normal” daily patient numbers and how fast the virus is spreading.
“Based on these analytics, we can estimate how many ICU beds will be needed across our system,” says Michael. “Hospitals are identifying rooms that can be converted into additional ICU capacity.”
HCA Healthcare’s network was one of the nation’s first to handle COVID-19, in San Jose, Calif. “Our experience provided real-time data, which the analytics team spun up within a week into an enterprise-wide tool to predict how many cases a hospital can expect, and the speed and severity of the outbreak,” says Michael. “This told us we needed more ICU beds.”
The result: 44 beds were quickly converted to meet the wave of patients. “We’re working around the clock to increase our capacity to handle the influx of patients,” he says. “There’s never been a more important time to be working in our profession.”


