Clinicians share their experiences caring for the growing number of unvaccinated patients as the number of COVID-19 hospitalizations increases across the nation and in our facilities.


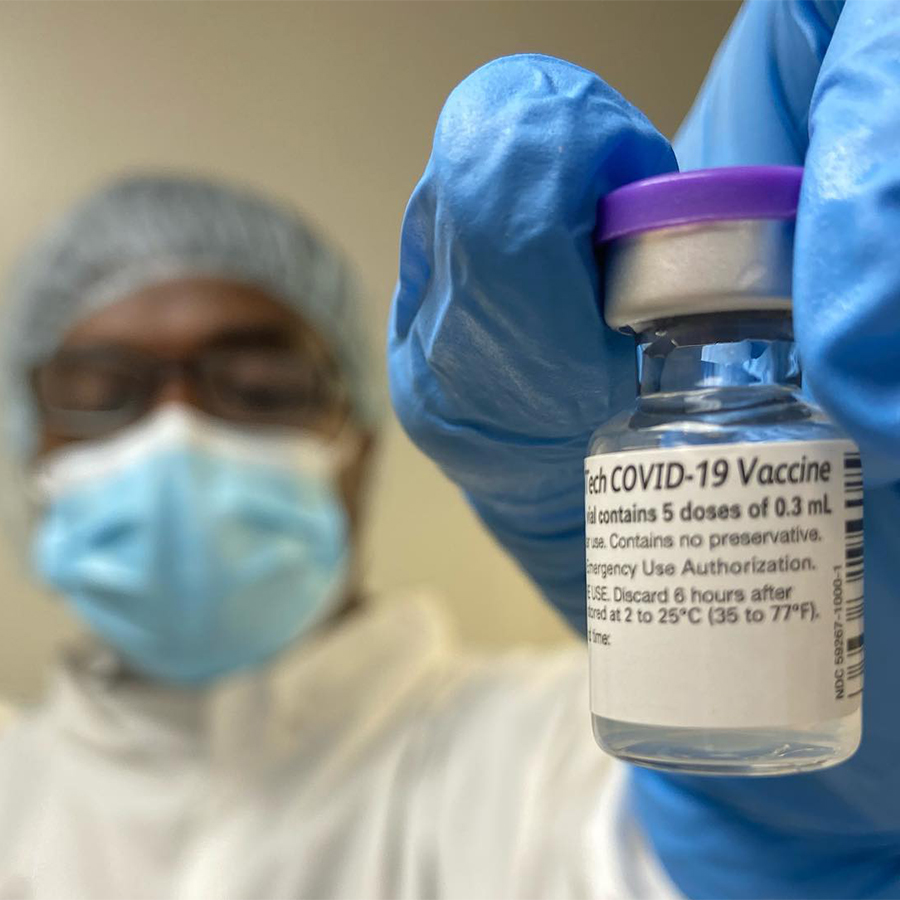
As COVID-19 vaccinations became available to colleagues last December, hope began to emerge from a year of unprecedented challenges. However, as the summer months come to an end and we begin moving toward the fall, the nation’s COVID-19 cases are again increasing. A recent news report shows that nearly all of the recent COVID-19-related hospitalizations and deaths have been among those who were unvaccinated.
In Tennessee, new COVID-19 cases rose 280% over 28 days by the end of July, says Sydney Hester, M.D., an infectious diseases physician at TriStar Centennial Medical Center in Nashville, Tennessee. This mirrors what is happening across the country: “This should make you stop and think, ‘Wait. Did I just hear that right?’”
Stephen Patterson, M.D., an emergency medicine physician at Riverside Community Hospital in Riverside, California, can also attest to alarming statistics at his own hospital.
The hospital serves a community that is predominantly Hispanic and Latinx, and there are some Native American and Black residents. These communities, he says, have been difficult to reach regarding vaccination education and guidance.
“We need to stress the importance of receiving vaccinations and continuing the best practices that we have been promoting with success throughout the course of this pandemic,” he says.
Dr. Patterson also urges the public to be proactive and responsible by getting vaccinated.
“I am asking you to reach out, contact your primary care providers, and approach the clinics and pharmacies that are offering these vaccinations so that you too can do your part,” he adds.
The frustration of battling the virus due to vaccine hesitancy is taking a toll on many healthcare workers.
In their own words, three HCA Healthcare colleagues discuss the current state of the pandemic at their respective hospitals, and the vital role of vaccines.

Sydney Hester, MD
Sydney Hester, M.D. Infectious Diseases Physician, The Frist Clinic at TriStar Centennial Medical Center, Nashville, Tennessee
The Virus Today
“We’re seeing more young patients, who make up the larger portion of the unvaccinated population. So now the hospitals are filled with these younger patients, anywhere from their mid-20s, 30s, up to 50s. Those are the people we’re taking care of in the hospital and in the ICU. Those are the patients who are dying. It’s not as much the 70- and 80-year-olds we were seeing last year, because most of them are vaccinated. It’s the younger population that is not.
“We’re seeing these cases go up because there is hesitancy and resistance to receiving the vaccines that are available. The current vaccines are remarkably effective against severe disease and death due to COVID-19, and that also includes the delta variant. It is a more contagious form of the virus, and it is more likely to cause severe illness and death. So, if you’re not vaccinated, you could be a pretty healthy person and still get very sick from COVID-19.”
Luders Michaud, Pharmacy Technician
Obstacles in the Way
“I’ve been in practice here at TriStar Centennial for 10 years. I went through all of this training, subspecialty training and an infectious diseases fellowship. Despite all of that, the knowledge, the skill set, the on-the-ground work for 10 years as a practicing physician — that doesn’t matter. People are listening to anyone other than their physicians.
“It’s really hard when you sit down, and you talk with a patient who’s known you for years. You’ve saved their life from an infection, and they say, ‘I’m not going to listen to you.’ It is a devastating obstacle.
“The hardest thing about this is that your decision is affecting the person sitting next to you on the bus. It’s affecting the person who’s sitting near you in your classroom or eating lunch with you that day. Your decision to not get a vaccine could lead to someone else having a tremendous change in their life, and they could die.”
"It’s really amazing what we can all do as a team and what we can do in medicine to bring someone on the brink of death to where they’re able to go home and be with their family again. It really is a miracle to see that unfold.— Sydney Hester, M.D. Infectious Diseases Physician, The Frist Clinic at TriStar Centennial Medical Center, Nashville, Tennessee.
Hope and Unity
“I’ll say from an intellectual standpoint, from an infectious diseases standpoint, just seeing this unfold and especially seeing the collegiality amongst physician scientists and people who are vaccine experts — to be able to work together and develop robust science and a vaccine that works — it’s just mind-blowing.
“You don’t get many vaccines that are 95% effective, like the Pfizer and Moderna vaccines. That’s amazing. If you had cancer and someone told you, ‘You have a 95% cure from taking a drug, you’d likely say, ‘Oh, my goodness. This is amazing!’ This truly is a miracle. It’s an answer to a prayer. This is science at its best.
“I applaud the scientific community and all the people who were behind the efforts of creating the vaccine and making sure it was safe and well done. And a well-designed study involving lots of age groups and different ethnic and cultural backgrounds was very important. That’s something that’s been really amazing to watch.
“The other important thing is the everyday work at the bedside, because that’s what I do. I see patients in the hospital and in the clinic. I’m 100% a clinician, working with my colleagues and seeing everyone support one another and be really encouraging and caring, holding one another up and asking, ‘How are you doing?’
The care that these nurses give these patients every day in the COVID-19 unit — I knew nurses were amazing before this, but just seeing them and the rest of the therapists and everyone working as a team is inspiring. You just get really invested in these patients, and you follow them for a long time. It’s really amazing what we can all do as a team and what we can do in medicine to bring someone on the brink of death to where they’re able to go home and be with their family again. It really is a miracle to see that unfold.
“When you step back and you get away from some of these other stresses, you think, ‘Wow, I really do have the most amazing job ever.’
“That is what keeps us going. That is what is bringing me to work every day. The fight is ongoing, and we all have to stick with it together.”
“The care that these nurses give these patients every day in the COVID-19 unit — I knew nurses were amazing before this, but just seeing them and the rest of the

Alma Rose Angeles, MSN, RN, CPST-1
Alma Rose Angeles, MSN, RN, CPST-1 Director of Nursing, Critical Care Services, HCA Healthcare, Sunrise Hospital & Medical Center, Las Vegas, Nevada
Separation From Loved Ones
“The most difficult thing we see at Sunrise Hospital with regard to the COVID-19 patient population is the separation of families from their loved ones. We saw this in the first wave of COVID-19, and there wasn’t anything we could do at that time. Now we’re seeing it again with these individuals of all ages coming in and experiencing the same suffering, if not worse than the first wave of the pandemic.
Also, there is suffering from the families’ perspective because they can’t be there. The families so much want to hold their loved ones’ hands — spouses, siblings, parents wanting to be there to provide emotional support and comfort.”
Survivor's Guilt
“During the first wave, there wasn’t anything we could do, but this time around, a lot of these experiences could have been avoided, prevented or mitigated had individuals gotten their vaccines.
“Their loved ones continue suffering after their loss — not even being able to say goodbye to them, not even having that closure of knowing what happened to them or letting their loved ones know that they were there at the very last moment that they took their very last breath on this earth.
“It can result in tremendous guilt, having not been the one to be there to hold their hand. Or worse, to have been the family member who came to a party or threw the party that encouraged the large gathering of individuals without vaccines that resulted in someone getting sick.”
Emotional Tolls and Sacrifices
“What we are seeing at Sunrise Hospital is both frustrating and disheartening. The fact that we’re finding that these individuals who are getting sick and dying are the result of not having the vaccination is extremely frustrating to our staff.
“Staff members are sacrificing their time from their families. A lot of them are picking up extra shifts to accommodate the volume of the surge that is coming in.
“I have nurses whose spouses or significant others take their children to their in-laws’ or another family member’s house to limit COVID-19 exposure, while they continue to work.
“Can you imagine mothers and fathers giving up time with their significant others and their children so that they can keep their families safe? That is a significant sacrifice they are making.”
"When people realize that they have people working with them and that we are working as a team, it motivates people and keeps people going.”— Stephen Patterson, M.D. Emergency Medicine and Emergency Medical Services, Riverside Community Hospital, Riverside, California.
Steve Patterson, M.D.
Stephen Patterson, M.D. Emergency Medicine and Emergency Medical Services, Riverside Community Hospital, Riverside, California
Supportive Environment
“The hospital’s administrative leadership has done a pretty fantastic job of maintaining levels of transparency and information sharing. Additionally, there’s this continued support of many within our medical community — physicians, nursing leadership and nursing staff; EMS; the hospital administrative leadership; and public health officials working to protect our community through education and the provision of PPE supplies. Just having those options available and the security of knowing that your work environment is safe for you is very important and a morale boost.”
Collective Efforts
“There’s also been a great deal of support from our community civic and religious leadership. This is really encouraging to us. There are community educators and leaders who are working tirelessly to enhance access to and education about vaccines. We’ve collaborated on a number of occasions to help share information.”
Remember the Team
“It is crucial and critical for our first responders, our healthcare providers, our frontline workers to continue every effort we can to maintain that sense of importance and relevancy, to maintain morale, boost spirits and keep people engaged in this fight.
“What we don’t want to see is people becoming exhausted, burned out or overwhelmed by what’s going on and what they see. I think that it is an unspoken tragedy throughout this pandemic that people have had to witness individuals dying alone, and that it has stressed the fabric of our ability to maintain a consistent morale and a consistent mindset throughout our caring for our patients.
“I think a big factor (in boosting morale) is maintaining a sense that we are working together as a team. And when people realize that they have people working with them and that we are working as a team, it motivates people and keeps people going.”


