Every Wednesday afternoon in a hospital conference room, Jorge Casas, MD, meets with a team of specialists: an oncologist, radiation oncologist, pathologist, radiologist, interventional radiologist, orthopedic surgeon, plastic surgeon, thoracic surgeon, and sometimes a vascular surgeon and surgical oncologist.
To treat rare sarcoma diagnoses, these are the doctors required.
Sarcomas are tumors that start in the bones or connective soft tissues, such as muscles, tendons and nerves. While they account for just 1% of all adult cancer — usually occurring in patients in their 50s, 60s and 70s — they make up 21% of childhood cancers.
Most of the time when you’re dealing with cancer, it’s a carcinoma, which lines the cells that form organs, such as the breast or lungs. Sarcomas on the other hand are exceedingly rare. “There are just a handful of us throughout the world that treat these tumors,” says Dr. Casas. Today, to receive cancer care for a sarcoma diagnosis, patients have to travel to a specialized cancer center for treatment. “Here in Dallas, 70% of my patients come from outside the Dallas-Fort Worth area. Parents drive or fly long distances for treatment, but this is to ensure they receive the highest level of care.”
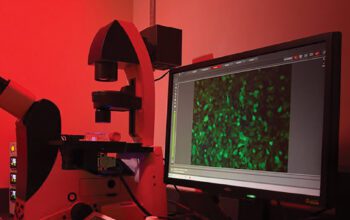
At this weekly sarcoma consensus conference, this team of doctors discuss one patient at a time, applying their knowledge and expertise to determine the next steps for treatment. “It really is a team sport,” says Dr. Casas. “We talk about diagnoses, present and review slides from biopsies, surgeries or imaging, and discuss how people are responding to chemotherapy and how to schedule surgeries.”