HCA Healthcare houses the largest burn and reconstructive surgery network in the nation.


Burn care and reconstructive surgery is an extremely rare specialty, with fewer than 150 burn centers in the United States. Some of the world’s leading burn care experts and specialists are affiliated with
HCA Healthcare, which has 15 centers across the country, including the nation’s largest, the Joseph M. Still Burn Center at Doctors Hospital in Augusta, Georgia. Our vast network of burn centers positions us as a leader in the field.
“We are incredibly proud of the dedication and excellence provided by our caregivers across all HCA Healthcare’s sites of care in caring for this complex, vulnerable population,” says Steven Manoukian, MD, senior vice president of HCA Healthcare Strategic Service Lines. “HCA [Healthcare’s] burn and reconstructive surgery network is the largest in the nation and delivers crucial care and life-changing support. Our coordinated efforts are impacting patients’ outcomes and lives in significant and meaningful ways.”
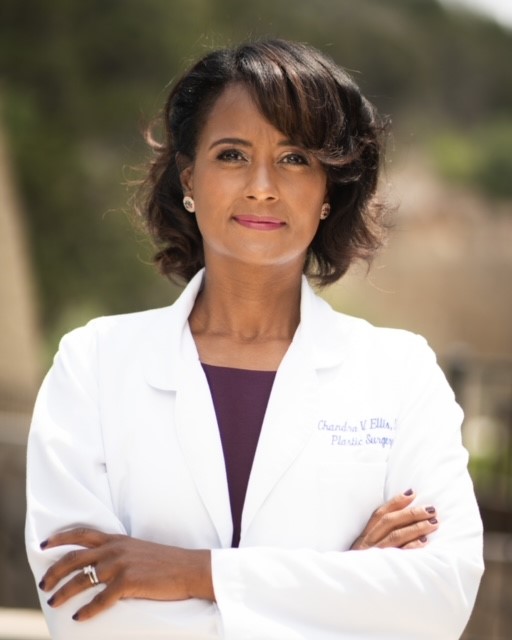
Chandra V. Ellis, MD, medical director for Methodist Hospital Burn and Reconstructive Center in San Antonio, Texas, has worked and trained with world-class burn and reconstructive surgeons throughout HCA Healthcare’s network.
“We can compare what other [HCA Healthcare] centers are doing so that we can improve outcomes. It gives us greater access to information and patients get better care,” she says.
This level of expertise also makes it possible for caregivers to share best practices and network with other burn specialists throughout HCA Healthcare and across the country.
Advancements and new technologies in burn care, the creative and technical skills required for treatment, and the intensely personal bonds formed with patients and their families are just a few of the reasons why HCA Healthcare burn care specialists love their jobs.

Michael Van Vliet, MD, the burn medical director at HCA Florida Blake Hospital, also says treatment requires his entire team’s involvement. His hospital is one of only six burn centers in Florida that has been verified by the American Burn Association as encompassing the highest level of care in all facets of burn care.
“A lot of times the physician gets the glory because we’re the doctor. However, it is truly a team effort,” he says. “The reason patients need to come to a burn center, especially an American Burn Association-verified one, is that we have all these team members that make it all possible for the patient to get through this.”

A Legacy of Care
The Joseph M. Still Burn Center at Doctors Hospital in Augusta, a 113-bed unit that treats thousands of patients with severe burns annually, is an established facility with a legacy in burn care.
The pioneering physician, Joseph M. Still, MD, was renowned in burn care and instrumental in establishing the center named in his honor, which is also known as the JMS Burn Center.
Zaheed Hassan, MD, is its current president. When he joined the staff 23 years ago, it was half the size it is now.
“If you love it, you’ll never leave it,” he says. “The smile on a patient’s face and the satisfaction of the patients — it is a perpetual source of happiness and energy.”
Dr. Hassan continues the legacy first established by Dr. Still and advanced by its former director, Dr. Fred Mullins, who passed away unexpectedly in 2020. Their work led to establishing Doctors Hospital of Augusta as a leader in burn care.
The Evolution and Future of Burn Care
Burn care has evolved greatly since the turn of the century. The greatest advancement within acute burn care has been regenerative medicine. There is now the capability to manufacture a patient’s skin from small biopsies in the lab.
“We’re essentially taking the small amounts of skin that they have left and using it to expand and apply to the burn to get them to heal,” says Dr. Van Vliet.
New products made from fish and cows also offer different templates of the dermis which can be used with regenerative medicine to eliminate the need for skin grafts.
Previously, surgeons treated patients with very deep burns by removing scar tissue and replacing it to create a new scar. New laser technology has transformed burn care and provided more hope to patients, says Dr. Van Vliet.

“We work with the scar that we have and manipulate it with laser technology rather than putting the patient through painful operations to excise scars, flaps, grafts and other things to reconstruct the scar,” he says.
A product that will soon be available in the U.S. is one that is currently being used in Europe. When applied to burn areas, it removes the dead skin, leaving behind only the healthy tissue.
“Right now, it’s hard to tease out which tissue is burned and what’s not as you get in depth of the burn. This gives you the exact level of debridement that you need to then reconstruct it,” says Dr. Van Vliet.
Other emerging developments in burn care are the use of 3D printing to replicate skin and artificial intelligence to assist in treatment. Artificial Intelligence could calculate data that could help guide care and predict healing times. This data would also help patients better prepare for their needs at home and work.
Dr. Van Vliet says HCA Healthcare’s extensive network is an asset when learning about new products and technologies. In addition to exchanging ideas and sharing experiences, he says there is an opportunity to use all their collected data for research leading to improved patient care.
A Balance of Skill, Creativity and Passion
Dr. Van Vliet, now entering his tenth year in practice, chose burn care because it encompasses all facets of plastic surgery, while also serving critically ill patients.
“When I was a general surgeon, I really enjoyed managing critically ill patients and getting them back to healthy life,” he says. “When I did my burn rotation as a plastic surgery resident, it really all came together.”
In medical school, he enjoyed the collaboration between physicians when coming up with creative solutions to problems.
“Plastic surgery just seemed like this unicorn where everyone was coming up with creative ways to solve a complex problem and there wasn’t necessarily one right answer,” he says.
A burn patient’s expected time in a hospital can be estimated by the percent of their injury. Burn patients have some of the longest hospitalizations due to complexity of the injury.
“It’s probably close to an oncology team in terms of the connectedness that we have with our patients,” Dr. Ellis says.
In addition to the physician, a burn care team includes occupational and physical therapists, dieticians, case managers, pharmacists and nurses.
When I was a general surgeon, I really enjoyed managing critically ill patients and getting them back to healthy life. When I did my burn rotation, as a plastic surgery resident, it really all came together.— Michael Van Vliet, MD, the burn medical director at HCA Florida Blake Hospital.

Madie Anderson found her calling through a chance encounter over her shift at a sushi restaurant. A customer was a charge nurse at HCA Midwest Health’s Research Medical Center in Kansas City, Missouri, and upon learning Anderson wanted to be a nurse, recommended she apply for an internship there. Anderson was accepted and toured the Grossman Burn Center at Research Medical Center while interning.
“The intersection between microbiology and the infection control that I was seeing in the burn center — it was just the perfect crossroads of everything for me,” she says.
Anderson has been an RN at the Grossman Burn Center for two years and has received accolades for her compassionate care, including a 2023 DAISY Award. She is fascinated with the pathophysiology of burns, infection control and the grafting process. Her knowledge and curiosity has helped her gain more confidence in performing the difficult task of dressing changes, which can be laborious and extremely painful for the patient.
The intersection between microbiology and the infection control that I was seeing on the burn unit — it was just the perfect crossroads of everything for me.— Madie Anderson,RN, the burn unit at Research Medical Center
“It’s really hard to go through that with a patient sometimes,” she says. “It definitely, at times, feels like we are the ones causing that pain, taking off dressings, putting them back on. I think understanding the pathophysiology of wounds has really helped.”
If a patient is unable to communicate, burn care staff often get to know their families very well. Such was the case of one of Anderson’s patients, a young man with extensive burns, which also led to multiple internal complications. His dressing changes sometimes took a couple of hours, and rooms must stay warm so that patients can maintain their body temperatures. Anderson sometimes emerged drenched with sweat. His family was deeply moved by her kindness and compassion. When he passed away, they invited her and other staff to join the memorial service.
“His family and I had gotten close, especially his parents, and they wanted to honor me for the work I did with him. It meant a whole lot to me,” she says.



