HCA Healthcare’s organ transplant program calls for the right leadership, evidence-based processes and the most advanced technology


There have been tremendous strides in transplant medicine since the first successful kidney transplant in 1954. HCA Healthcare’s transplant and dialysis programs can keep patients with failing organs living longer, even giving them new lives via organ transplants.
“It comes down to three things — people, process and technology — and the ability to have the right people, the right leadership,” says James Pittman, HCA Healthcare’s assistant vice president of Transplant and Dialysis Services. “Physician leadership in transplant is so important.”
Methodist Hospital Specialty and Transplant in San Antonio, Texas, exemplifies HCA Healthcare’s transplant expertise. Led by Dr. Adam Bingaman, HCA Healthcare’s national medical director of solid organ transplant, it is the world’s largest live-donor kidney transplant center, with 429 live-donor kidney transplants in 2020-2021.
Set Up for Success
Organ transplants often occur toward the end of a medical journey. HCA Healthcare continued its robust transplant program, even while managing the challenges of a pandemic, through a full commitment to organ procurement.
Procurement efforts have led to a greater percentage of living donor transplants, a key component in predicting long-term transplant success. Nationally, of the 18,799 kidney transplants in 2021, 24.2% involved living donors, while 75.8% were from deceased donors
Conversely, of HCA Healthcare’s 1,103 kidney transplants, close to 35% involved living donors, and 65% were from deceased donors. Additionally, there have been policy changes at the federal level for the Organ Procurement and Transplantation Network (OPTN), the organization that governs the bylaws and rules related to transplant and organ allocation, explains James.
HCA Healthcare, he says, has worked diligently to expand the exchange of information with the organ procurement organizations, “which then enhances their ability to recover more organs more efficiently.”
That’s critical, says James, because while OPTN and the United Network for Organ Sharing, which manages the national transplant waiting list, receive more than a million referrals for potential donors, only roughly 30,000 patients become organ donors.
Finding the Right Match
Organs such as kidneys, whether from a deceased donor or a living one, come in a predictably wide range of quality. Some are pristine, while others can be quickly rejected. The majority fall into a middle ground and may or may not be adequate, depending on how well the organ pairs with the patient.
“What’s important is matching that organ with the recipient and making sure, based on our experience and the experience of the community, that this type of organ will actually do well in this type of patient,” says James.
HCA Healthcare routinely hosts forums where physicians can confer and network with each other, which have been most impactful in leveraging best practices.
“That’s taking the best practices that have been tried and true and tested at Methodist Specialty and Transplant Hospital and understanding how they do it,” James says.
Living Donor Transplants
“It’s much easier to do a transplant from a deceased donor, because the hospital is not involved in the procurement of that deceased-donor organ,” says James.
With a deceased donor, the organ typically arrives via commercial airline, packed in ice, underscoring the value of transportation. But the facility transplant team is solely responsible for the recipient.
When it comes to living donor transplants, timing is critical. With a living organ transplant, the team must coordinate between both the donor and recipient.
“Our transplant teams work closely together to provide the best possible care for the patient during the operation and post-transplant,” says James.
“If you don’t have a team that’s just entirely focused on really maximizing the opportunity of living donation, you won’t meet or match the success that Methodist has had. And that’s how they’ve done it,” he adds.
Access to Success
Access to care can be a key factor in receiving a transplant. Patients often assume they’re not eligible if they live too far from major medical centers.
“We’re primarily in community-based hospitals, so we’re not necessarily in the giant downtown medical centers that are where you often see transplant programs,” says James.
“We routinely partner with the end-stage renal disease community, with primary care and dialysis centers, and provide education directly to patients about end-stage renal disease,” he adds. “We continue to look for ways in which we can use technology to identify potential patients who might be in need.”
Learn more about living organ donation through the private, nonprofit United Network for Organ Sharing (unos.org).
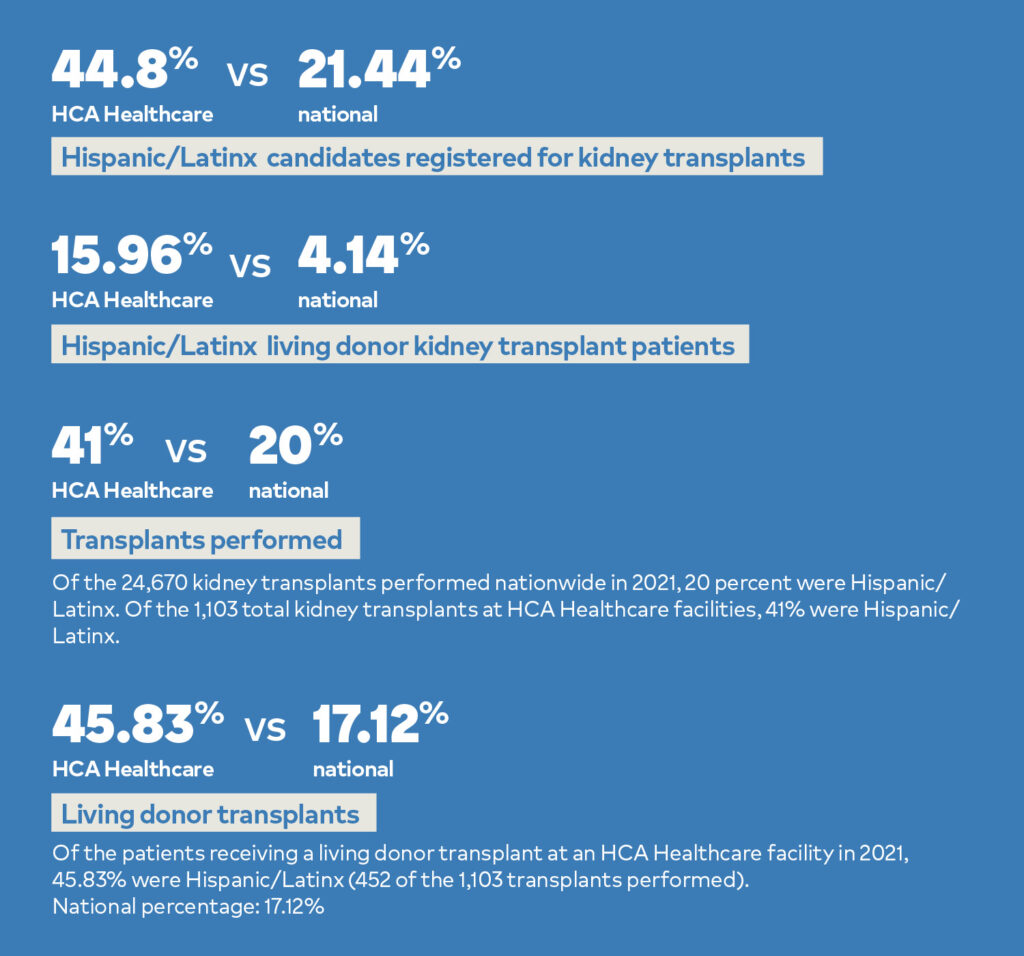
Serving Hispanic/Latinx Transplant Patients
With the groundbreaking work at Methodist Specialty and Transplant Hospital in San Antonio setting the pace, HCA Healthcare has emerged as a leader in providing access to kidney transplants to the country’s Hispanic/Latinx population. More importantly, of those 1,103 transplants at HCA Healthcare facilities involving a living donor kidney transplant, 15.96% (176) were Hispanic/Latinx patients, compared to 4.14% nationally. That’s a significant difference, given the superior outcomes of kidney transplants with a living donor.