(Part 1)
This is the first story in a two-part series. You can read the second story here.

(Part 1)
This is the first story in a two-part series. You can read the second story here.
HCA Healthcare’s clinical trials led to groundbreaking and transformative technology.
Innovation is the lifeblood of modern medicine, reflecting a consistent search for new technologies and refined techniques that improve patient care. Talented clinicians across our network use their expertise to transform innovative ideas into the industry-wide best practices and medical advancements of tomorrow through a critically important process: clinical trials.
“A clinical trial is a formal study for which the patient has consented and enrolled, and there’s a specific aim or goal of the study,” explains John Day, MD, a cardiac electrophysiologist at St. Mark’s Hospital in Salt Lake City, Utah, and physician executive of HCA Healthcare’s Mountain Division Cardiovascular Program.
According to Dr. Day, who specializes in diagnosing and treating heart rhythm disorders, some clinical trials are sponsored by the National Institutes of Health (NIH) or an organization like the American Heart Association. Other times, trials are supported by an industry that wants to test a new technology to bring it to market.

Trials adhere to a rigid set of rules, require participation from numerous facilities and must be closely monitored by a panel of “referees” to generate the data required for sound conclusions, says Dr. Day. “You’ve got to test the therapies to prove they’re going to work and be efficacious, and with significant benefit and minimal risk of harm.”
Sybil Hyatt serves as AVP of Site Operations for HCA Healthcare’s Research Institute.
She says clinical trials require a significant financial investment since some studies, such as those investigating structural cardiac issues, involve a
10-year follow-up on initial results.
“That’s a big commitment,” says Hyatt, noting HCA Healthcare’s scale, as one of the nation’s largest healthcare networks, provides the stability to take on that obligation.
Studies led by HCA Healthcare colleagues are producing pioneering results in an emerging technique — pulsed field ablation — which gives cardiac patients a new lease on life.
Atrial fibrillation, or AFib, is the most common type of heart arrhythmia, where the heart’s upper chambers beat quickly and irregularly. This can disrupt the normal flow of blood through the heart, which can result in a host of medical issues, potentially leading to blood clots, stroke and other heart-related complications.
“You have complete electrical chaos of the two upper chambers of the heart,” explains Dr. Day. In most cases, a rapid, irregular heartbeat can cause fatigue and shortness of breath with exertion. But it also could cause chest pain, palpitations, dizziness, lightheadedness and panting.
According to Dr. Day, AFib increases your risk of stroke five times and doubles your risk of heart failure and dementia. “The brain doesn’t work as well when you’re in AFib. Basically, your brain, your kidneys, your heart, they don’t like it. Organs like nice, steady blood flow, not the chaos induced by AFib.”
Unfortunately, studies show that one in four Americans will have at least one episode of AFib at some point in their lives. “The older you get, the higher your risk,” says Dr. Day. “Being Caucasian puts you at higher risk. Being a couch potato puts you at risk, or being an exercise maniac puts you at risk. Obesity is a huge risk factor. High blood pressure is a big risk factor. Alcohol can be a risk factor. Sleep apnea, sleep deprivation, stress, these all play roles.”
“The beautiful thing about pulsed field ablation is it saves the rest of the tissue. It’s very safe, and it doesn’t knock out tissue indiscriminately. This is groundbreaking, transformative new technology for treating atrial fibrillation."— John Day, MD, Cardiac Electrophysiologist, St. Mark’s Hospital, Salt Lake City, Utah
Physician Executive of HCA Healthcare’s Mountain Division Cardiovascular Program
Until recently, treatment for AFib typically involved one of two main strategies: medications to control the heart rate or rhythm, or catheter ablation to disrupt the abnormal electrical signals causing the arrhythmia. Contrary to popular belief, a pacemaker does not treat AFib itself — except in rare cases where it’s used in combination with other procedures. “Pacemakers do nothing for atrial fibrillation,” explains Dr. Day. “They’re designed to treat slow heart rhythms. All a pacemaker does is keep the heart from going too slow.”
Both medications and ablations have their limitations. “We don’t have great long-term medications for atrial fibrillation,” says Dr. Day. “In many patients, even when medications do work, they often only maintain normal rhythm for a year or two. Over time, the disease can progress to the point where the antiarrhythmic medications are no longer effective at keeping the heart in rhythm.”
Meanwhile, the two most widely used ablation treatments historically — radiofrequency ablation (RFA) and cryoablation (or cryotherapy) — have helped many patients with atrial fibrillation, but they can occasionally damage surrounding tissues. RFA uses heat, while cryoablation uses extreme cold to target and disable areas of heart tissue responsible for abnormal electrical signals.
“Radiofrequency is like a microwave,” says Dr. Day. “It uses heat to create small, controlled scars in the heart that stop abnormal rhythms. Cryoablation, on the other hand, freezes the tissue until it stops conducting. Both approaches can be effective, but depending on the location, they may also potentially damage nearby structures.”
Enter pulsed field ablation (PFA) — a new approach that uses non-thermal electrical pulses (a process called electroporation) to selectively target the electrically active cells that cause atrial fibrillation. Rather than heating or freezing the tissue, PFA creates microscopic pores in the membranes of heart muscle cells, disrupting their ability to conduct erratic electrical signals — while sparing surrounding tissues like nerves, blood vessels and the esophagus.
“The beautiful thing about pulsed field ablation is how tissue-selective it is,” says Dr. Day. “It spares smooth muscle, small blood vessels, nerves — even the microvascular system. It’s very safe and doesn’t damage tissue indiscriminately. This is truly groundbreaking technology for treating atrial fibrillation — great news for people who are suffering.”

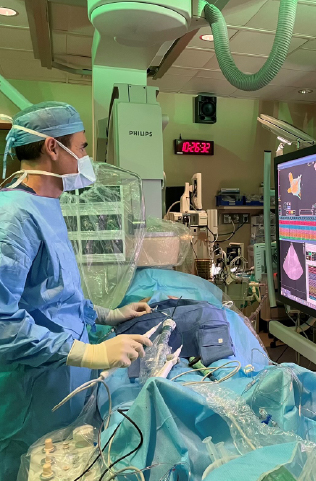
The EP lab team at St. Mark’s Hospital in Salt Lake City, Utah, celebrates their first pulsed-field ablation.