HCA Healthcare’s repository of colleague expertise, valuable partnerships, access to resources and proven track record of responding to disasters ensures continuity of patient care, even in unprecedented times.


Katrina. Harvey. Beryl. Ian. These unforgettable names are infamous in hurricane history for the magnitude of their aftermath. In 2024, Hurricanes Helene and Milton joined this list.
Hurricane Helene, which impacted Florida, Georgia, the Carolinas, Tennessee and Virginia as a Category 4 storm, is the second deadliest hurricane — behind Katrina in 2005 —to make landfall this century in the continental U.S.. In western North Carolina, catastrophic flooding from Helene wiped out entire communities, destroyed the infrastructure of multiple towns and caused more than 200 deaths.
Two weeks later, Milton struck Florida as a Category 3 storm that spawned roughly four dozen tornadoes throughout the state and caused massive flooding in central and west Florida. Throughout both disasters,
HCA Healthcare stood ready with the resources needed to provide uninterrupted patient care, and to support our colleagues and communities. Our national network of resources, including colleagues, supplies, vendor relationships and more, allowed us to respond immediately in a way that only HCA Healthcare can. Our scale sets us apart, and the skill and dedication of our people makes our crisis response possible.
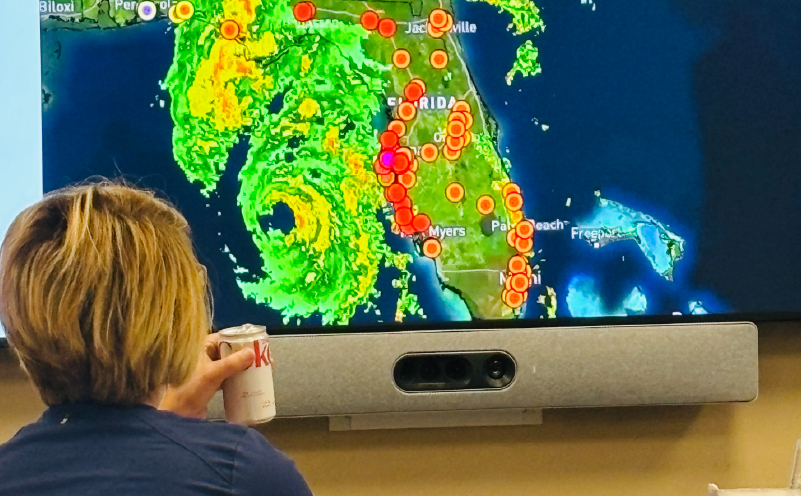
As Hurricane Milton moved across Florida, Georgia and into North Carolina, our emergency operations teams kept a close eye on the storm’s impact on HCA Healthcare facilities to ensure critical resources could be quickly deployed to support our patients and colleagues.
Preparing for the unpredictable
Before Hurricane Helene made landfall in Florida on Sept. 26 with record-breaking surges, HCA Healthcare’s Enterprise Emergency Operations Center (EEOC) in Nashville, Tenn. had been monitoring the storm as it gained strength in the Caribbean. Our West and North Florida divisions began de-risking critical patients, evacuating hospitals and preparing facilities to shelter in place by Sept. 23. Incident Response Teams were deployed to Florida the very next day. Meanwhile, Garima K. Stack, South Atlantic Division vice president of Quality & Patient Safety, Dr. B. Patrice Vance, West Florida Division vice president of Clinical Operations and Quality and senior leadership at Mission Health were leading emergency response operations across their respective divisions.
HCA Healthcare’s EEOC introduced Incident Response Teams in 2020. Today, hundreds of members across HCA Healthcare are trained annually on how to effectively respond to events impacting patient care or colleague wellness. All team members are part of the Enterprise Emergency Operations Program, made up of corporate, division and hospital-based clinicians, leaders and executives from numerous states across our organization who are cross-trained as incident response personnel during events such as hurricanes.
When disasters escalate, our priority is first and foremost the safety of patients and colleagues. A secure infrastructure plays a key role in ensuring the safety of those involved. A 6,500 square-foot flood control barrier was deployed at HCA Florida Pasadena Hospital. While generators and fuel trucks were delivered, colleagues and first responders began to arrive at facilities across Florida and Georgia.
In the days leading up to Helene’s arrival, the EEOC began paying close attention to North Carolina as well. Nearly three months’ worth of precipitation fell across the western North Carolina mountains over just three days. HCA Healthcare’s weather contractor, StormGeo, which provides weather forecasts, alerts, and other services to guide decision-making, indicated the potential for massive flooding in the area.
We are incredibly fortunate to be part of HCA Healthcare, where there is no shortage of sister facilities for us to partner with for guidance and best practices.— Greg Lowe, President, North Carolina Division

At HCA Florida Pasadena Hospital, flood control barriers were established around the facility before the storm even began, ensuring rising waters were kept from critical areas of the hospital.
In preparation, detailed hurricane and flooding playbooks were distributed to HCA Healthcare facilities in and around western North Carolina, and an Incident Response Team was deployed in preparation for what might be in store.
“We are incredibly fortunate to be part of HCA Healthcare, where there is no shortage of sister facilities for us to partner with for guidance and best practices,” says Greg Lowe, president of HCA Healthcare North Carolina Division, which includes Mission Health in Asheville.
It soon became clear that Helene was going to leave an unprecedented impact. More than 20 subsequent tornadoes were reported across five states, four million people were left without power and nearly 230 fatalities were reported. An excess of 12 inches of rain fell in Augusta, Georgia and more than two feet of rain deluged western North Carolina, where homes, automobiles and people were swept away in floods, mudslides and landslides. Much of the damage from Helene occurred in areas that rarely experience storms of that magnitude and, therefore, didn’t have the experience or response mechanisms at the ready to respond. In addition to power outages, Helene also destroyed cellphone towers, leaving families unable to communicate with loved ones or even call for help. Floodwaters burst through pipes and pump stations, causing catastrophic damage to a major reservoir. Extensive damage to water systems left more than 100,000 people without potable water for weeks, and even into November.
Michael Wargo, vice president of Enterprise Emergency Operations, explained how an advanced level of planning is required when a community’s water and communication systems are threatened.
“When you think about the loss of those utilities and the cascading (effects) that it had, I don’t know that any of us anticipated the broad impact to the community,” Michael says. “From an internal perspective, we had all the T’s crossed and I’s dotted from a preparedness standpoint. But when you have a complete wipeout of a community water system, never did any of us think that we would be trucking in 30-plus tanker trucks per day just to support the hospital system.”
Mission Hospital in particular became a critical area of focus, as any disruption of services would be a major disruption to the entire region. Mission Hospital, which serves 18 of the 27 western North Carolina counties touched by Helene, became a beacon of hope in the community. Residents from across the region gravitated to Mission Hospital, even if they had no need for medical attention, because they knew they could find food, potable water and a Wi-Fi signal to reach loved ones.
They are this magical team – you give them any task, they have the right skill set and they figure it out.— -Michael Wargo, Vice President, Enterprise Emergency Operations
To maintain hospital operations, HCA Healthcare deployed:
- Tanker trucks to provide water
- Engineers from HCA Healthcare facilities across the country to develop innovative solutions including new wells, to allow access to water
- Portable showers and laundry units for colleagues without access to water
- Generators and tanker trucks for hotels throughout Asheville where colleagues and their families stayed while supporting Mission Health or while displaced during the storm
These efforts were made possible through established relationships, partnerships and our HealthTrust line of business.
“The amazing part of this is that we have the contracts, the plans, the relationships to be able to do this and that’s the Herculean effort that every person involved in our storm preparation and response activity plays a pivotal role in,” Michael says. “When you look at our supply chain and the depth of resources we have, that’s really a major component of our success.”
Building a team of the very best
Incident Response Team members represent trained staff across all 15 divisions. The EEOC solicits applicants annually. Applicants are identified by their division EOCs or through interactions with current Incident Response Team members during deployments or through preparedness activities throughout the year. Applicants are selected for their specific expertise in areas such as plant operations, safety and security, emergency management and behavioral health. A Downtime Response Team of IT and communication experts also manages downtime response. Additionally, a NICU Incident Support Team of nurses, respiratory therapists and flight paramedics assists with NICU patient transport.
Once selected, Incident Response Team members attend an annual in-person weeklong training and participate in virtual readiness meetings throughout the year. They volunteer on deployments, with the support of their supervisors.

As the storms approached the coast, local Emergency Operations teams like those at Lake City Hospital in Florida began to gather and prepare.
Incident Response Teams: The special forces in healthcare
When an HCA Healthcare facility faces a disaster, its leaders are supported by a team of experts from across the organization. Enterprise Emergency Operations, senior executives and Incident Response Teams all serve alongside one another to assist with preparations, troubleshooting and operations throughout the disaster.
Hospital leadership is on the ground and at the front lines during these events day and night. Having a fresh team ready to step in and assist goes a long way during challenging times. Incident Response Team members include managers with expertise in plan operations, safety and security, as well as ER nursing to help strategize throughput to meet a community surge.
“I am so grateful for the specialists from our Incident Response Teams and the assistance they have provided to our hospitals since the storm, including the management of our command center,” says Greg Lowe, president of HCA Healthcare North Carolina Division.
Incident Response Teams can give the right assessment and provide the right resources during an emergency. Their value was especially demonstrated in Asheville. Team members came from across the country, including nurses, engineers, design and construction teams, and supply chain leaders. Engineer and construction team members figured out how to get water from the tanker trucks through the faucets at Mission Hospital. They display the full spectrum skill sets of colleagues from across the country who are trained to help facilities get through a crisis no matter the challenge — engineering, leadership, supply chain or clinical.
Forty-two Incident Response Teams — a total of 572 colleagues from across the country — were deployed for Helene and Milton. Six teams shifted between Florida and Georgia for Helene, while 15 served in Asheville. Twelve teams went to Florida for Milton and nine supported the Enterprise Emergency Operations Center at corporate headquarters.
Incident Response Teams supported in various ways, including:
• Assisting facility leadership in making critical decisions and organizing their incident management and facility reporting structures
• Assisting with patient evacuations and flood control barrier
• Coordinating cargo helicopter supply missions for outlying hospitals in North Carolina
• Conducting post-storm damage assessments for impacted hospitals, physician practices, urgent care centers and freestanding emergency departments
• Establishing mini-marts and colleague support centers and procuring urgently needed supplies on the ground
• Helping establish a modular, free-standing emergency department at HCA Florida Largo Hospital
• Providing colleagues with behavioral health services and therapy dog visits in North Carolina


